Background
Cervical disc disorders encountered in physiatric practice include herniated nucleus pulposus (HNP), degenerative disc disease (DDD), and internal disc disruption (IDD). (See image below and Image 1.) HNP implies extension of disc material beyond the posterior margin of the vertebral body. Most of the herniation is made up of the annulus fibrosus. DDD involves degenerative annular tears, loss of disc height, and nuclear degradation. IDD describes annular fissuring of the disc without external disc deformation. Cervical radiculopathy can result from nerve root injury in the presence of disc herniation or stenosis, most commonly foraminal stenosis, leading to sensory, motor, or reflex abnormalities in the affected nerve root distribution.1,2
Sagittal magnetic resonance imaging (MRI) scan demonstrating cervical intervertebral disc protrusions at C3-C4 and C7-T1.
Understanding cervical disc disease requires basic knowledge of anatomy and biomechanics. The intervertebral disc absorbs shock, accommodates movement, provides support, and separates vertebral bodies to lend height to intervertebral foramina. The disc consists of an eccentrically located nucleus pulposus and a surrounding annulus fibrosus separating each segmental level between the C2-T1 vertebrae. No disc exists between C1 and C2, and only ligaments and joint capsules resist excessive motion. Disc degeneration and/or herniation can injure the spinal cord or nerve roots and result in stenosis3 and/or myofascial pain.
Pathophysiology
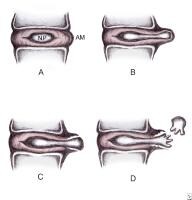
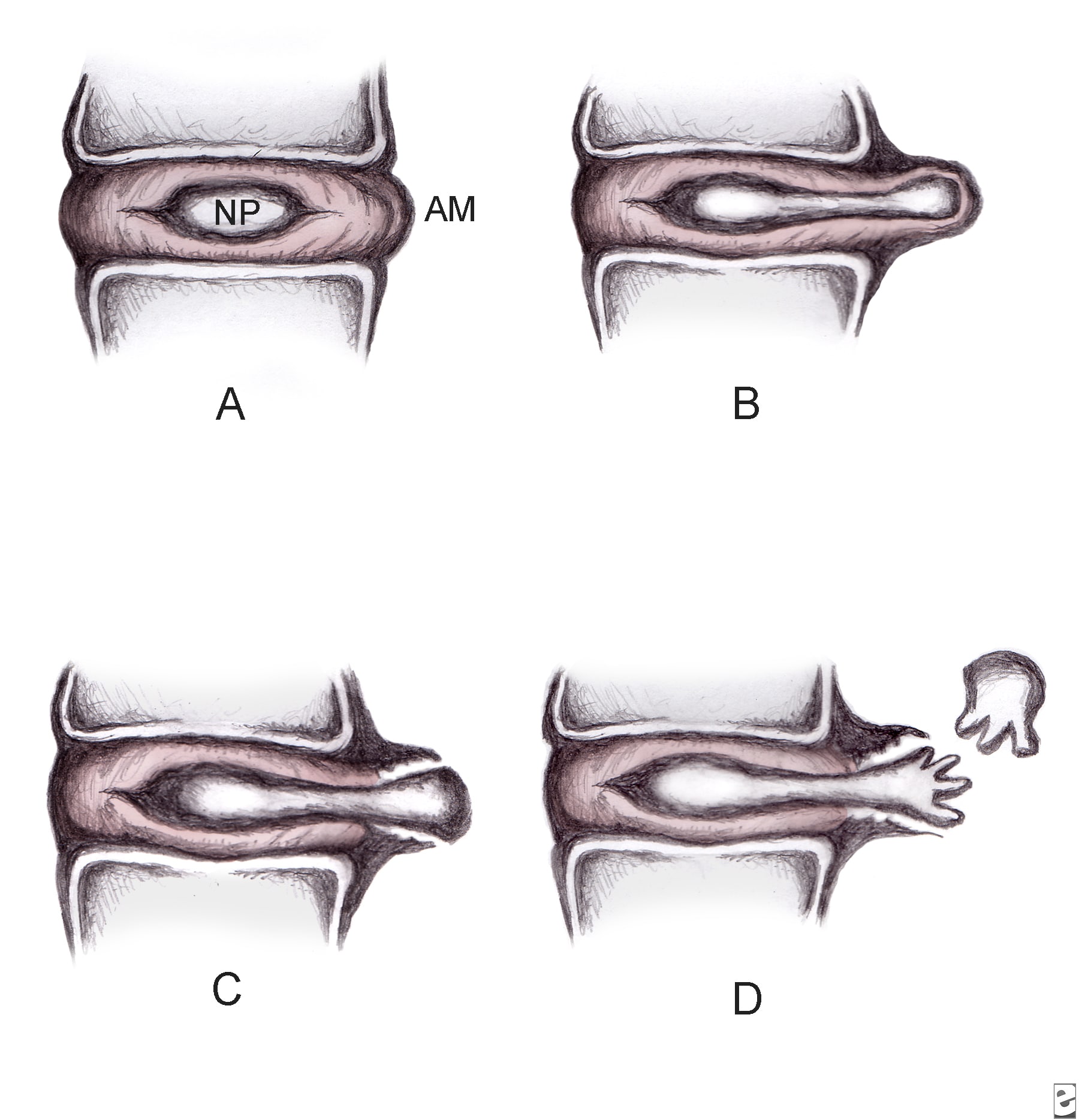
Manifestations of HNP are divided into subcategories by type (ie, disc bulge, protrusion, extrusion, sequestration). Disc bulge describes generalized symmetrical extension of the disc margin beyond the margins of the adjacent vertebral endplates. Disc protrusion describes herniation of nuclear material through a defect in the annulus, producing a focal extension of the disc margin. Extrusion applies to herniation of nuclear material resulting in an anterior extradural mass attached to the nucleus of origin, often via a pedicle. Disc sequestration refers to separation of material from the disc, which ultimately comes to lie in the spinal canal. (See images below and Images 1-3, 8.)
Disc herniation classification. A: Normal disc anatomy demonstrating nucleus pulposus (NP) and annular margin (AM). B: Disc protrusion, with NP penetrating asymmetrically through annular fibers but confined within the AM. C: Disc extrusion with NP extending beyond the AM. D: Disc sequestration, with nuclear fragment separated from extruded disc.
Axial magnetic resonance imaging (MRI) scan (C3-C4) demonstrating left-sided posterolateral protrusion of the nucleus pulposus with compression of the cerebrospinal fluid.
Sagittal magnetic resonance imaging (MRI) scan demonstrating cervical intervertebral disc protrusions at C3-C4 and C7-T1.
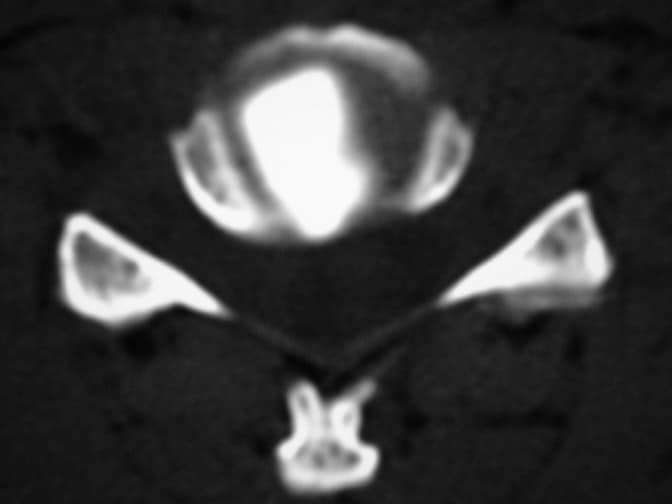
Postdiscography axial computed tomography (CT) scan demonstrating right posterolateral subligamentous protrusion.
Herniation typically occurs secondary to posterolateral annular stress. Herniation rarely results from a single traumatic incident. Acute traumatic cervical HNP serves as a major etiology of central cord syndrome. The C6-C7 disc herniates more frequently than discs at other levels.
Acute disc herniation causes radicular pain through chemical radiculitis in which proteoglycans and phospholipases released from the nucleus pulposus mediate chemical inflammation and/or direct nerve root compression. Interleukin 6 and nitric oxide are also released from the disc and play a role in the inflammatory cascade. The chemical radiculitis is a key element in the pain caused by HNP as nerve root compression alone is not always painful unless the dorsal root ganglion is also involved. Herniation may induce nerve demyelination with resulting neurologic symptoms. Cervical HNP may be resorbed during the acute phase. Indeed, studies documenting frequent herniation resorption and correlating herniation regression with symptom resolution support conservative treatment of cervical radicular pain.
A rare trauma-induced high cervical (C2-C3) HNP syndrome manifests as nonspecific neck and shoulder pain, perioral hypesthesia, more radiculopathy than myelopathy, and more upper limb motor and sensory dysfunction than lower limb symptomology. Decreased middle and/or lower cervical spine mobility from spondylosis, with consequent overload at higher segments, may precipitate high cervical disc lesions in older patients. A retro-odontoid disc may result from an upwardly migrating C2-C3 HNP. Some case reports describe cervical HNPs causing Brown-Séquard syndrome, as well as atypical nonradicular symptoms in patients with congenital insensitivity to pain.
Cervical radiculopathy results from mechanical nerve root compression or intense inflammation (ie, chemical radiculitis). Specifically, nerve root compression may occur at the intervertebral foraminal entrance zone at the narrowest segment of the root sleeve anteriorly by disc protrusion and uncovertebral osteophytes and posteriorly by superior articulating process, ligamentum flavum, and periradicular fibrous tissue.4 Decreased disc height, as well as age-related foraminal width decrease from inferior Z-joint hypertrophy, may impinge subsequently on nerve roots. The cervical region accounts for 5-36% of all radiculopathies encountered. Incidence of cervical radiculopathies by nerve root level is as follows: C7 (70%), C6 (19-25%), C8 (4-10%), and C5 (2%).
The most common cause of cervical radiculopathy is foraminal encroachment (70-75%). The cause is multifactorial, including degeneration of the discs and the uncovertebral joints of Luschka and the zygapophyseal joints. In contrast to lumbar spine disorders, HNP in the cervical spine is responsible for only 20-25% of radiculopathies.
Cervical DDD most commonly is due to age-related changes, but the condition also is affected by lifestyle, genetics, smoking, nutrition, and physical activity. Degenerative disc changes observed on radiographs may reflect simple aging and do not necessarily indicate a symptomatic process.
The disc begins to degenerate in the second decade of life. Circumferential tears form in the posterolateral annulus after repetitive use. Several circumferential tears coalesce into radial tears, which progress into radial fissures. The disc then disrupts with tears passing throughout the disc. Loss of disc height occurs with subsequent peripheral annular bulging. Proteoglycans and water escape through fissures formed from nuclear degradation, resulting in further thinning of the disc space. Vertebral sclerosis and osteophytic formation ultimately follow.5
IDD describes pathologic annular fissuring within the disc without external disc deformation. This disorder results from trauma-related nuclear degradation, cervical flexion/rotation-induced annular injury, or whiplash. The innervated outer disc annulus serves as a major pain generator. DDD ultimately may progress to IDD.
Frequency
United States
HNP may be observed with magnetic resonance imaging (MRI) in 10% of asymptomatic individuals aged younger than 40 years and 5% of those older than 40 years. Degenerative disc disease (DDD) may be observed with MRI in 25% of asymptomatic individuals aged less than 40 years and 60% of those aged more than 40 years. The true incidence and prevalence of cervical radiculopathy is uncertain; however, 51% of adults experience neck and arm pain at some time. In a population-based study in Rochester, Minn, the annual incidence of documented cervical radiculopathy for men and women from all causes was 107.3 and 63.5 cases per 100,000 population, respectively.6
International
A study from Italy in 1996 reported a prevalence of cervical spondylotic radiculopathy as 3.5 cases per 1000 people.7
Mortality/Morbidity
Occasionally, an acute HNP can herniate centrally and cause a myelopathy. This can manifest as hyperreflexia, positive pathologic reflexes (such as Babinski and Hoffman signs), and sphincter disturbances. If left untreated, the effects can be irreversible.
Sex
Kelley suggests that the male-to-female incidence of cervical disc herniation is approximately 1:1.8 Marchiori and Henderson cite women as reporting higher disability with increasing levels of DDD than men.9
Age
HNP typically affects younger patients (ie, <40>40 y).
Clinical
History
- Pertinent history should include the following information:
- Information about pain onset (eg, abrupt onset suggests acute injury)
- Time since injury
- Mechanism of injury
- Percentage of axial versus peripheral pain (eg, 90% neck pain vs 10% upper limb)
- Review of systems to uncover possible systemic illness (eg, fever suggests infection, weight loss suggests malignancy).
- Discogenic pain without nerve root involvement typically is vague, diffuse, and distributed axially.
- Pain referred from disc to upper limb usually is nondermatomal.
- Activities that increase intradiscal pressure (eg, lifting, Valsalva maneuver) intensify symptoms. Conversely, lying supine provides relief by decreasing intradiscal pressure.
- Vibrational stress from driving also exacerbates discogenic pain.
- Depending on whether primarily motor or sensory involvement is present, radicular pain is deep, dull, and achy or sharp, burning, and electric.
- Such radicular pain follows a dermatomal or myotomal pattern into the upper limb.
- Cervical radicular pain most commonly radiates to the interscapular region, although pain can be referred to the occiput, shoulder, or arm as well.
- Neck pain does not necessarily accompany radiculopathy and frequently is absent.
- Patients may present with distal limb numbness and proximal weakness in addition to pain. Atrophy may be present.
- A study has demonstrated cervical HNP-induced thermal changes (ie, thermatomes) in specific upper extremity distributions.
- Mechanical stimulation of cervical nerve roots has shown that the distribution of referred radicular symptoms (ie, dynatome) may be different from sensory deficits outlined by traditional dermatomal maps.
Physical
- The patient with radicular pain also displays decreased cervical range of motion (ROM).
- Pain is exacerbated by neck extension and rotation or by Spurling maneuver (patient's neck is extended, laterally bent, and held down) designed to elicit radicular symptoms.
- Pain improves with neck flexion or with abduction of the symptomatic upper limb over the top of the head (abduction sign).
- Decreased sensation to pain, light touch, or vibration may be present in the distal upper limb. Proximal limb weakness manifests when significant motor root compromise exists, but this symptom must be differentiated from pain-related weakness.
- Diminished or absent reflexes corresponding to the root level may be present.
- Increased upper and lower limb reflexes or other upper motor neuron signs suggest myelopathy and mandate aggressive diagnostic evaluation.
- The patient with discogenic pain without nerve root involvement demonstrates decreased cervical ROM, normal neurologic examination, and possible pain exacerbation with axial compression and pain alleviation with distraction.
- Myofascial tender or trigger points, which may be primary in origin or secondary to other pathologic processes, commonly are palpable.
- Tenderness with posteroanterior mobilization may suggest disc pathology.
Causes
- HNP results from repetitive cervical stress or, rarely, from a single traumatic incident. Increased risk may accrue because of vibrational stress, heavy lifting, prolonged sedentary position, whiplash accidents, and frequent acceleration/deceleration.
- DDD is part of natural aging, but it is also a consequence of poor nutrition, smoking, atherosclerosis, job-related activities, and genetics.
- IDD can result from cervical trauma, including whiplash, cervical flexion/rotation injury, and repetitive use.
- Cervical radiculopathy results from nerve root compression secondary to herniated disc material, stenosis, or proteoglycan-mediated chemical inflammation released from discs. Smoking and certain occupational activities also predispose patients to cervical radiculopathy





I've been browsing online more than 2 hours today, yet I never found any interesting article like yours. It is pretty worth enough for me. Personally, if all website owners and bloggers made good content as you did, the net will be much more useful than ever before.
ReplyDeleteFeel free to surf to my web page; best acne treatments (http://www3.rn.Ac.th)
I could not resist commenting. Very well written!
ReplyDeletemy website adult acne treatment
Write more, thats all I have to say. Literally, it
ReplyDeleteseems as though you relied on the video to make your
point. You clearly know what youre talking about, why waste your intelligence on
just posting videos to your site when you could be giving us something enlightening to read?
Feel free to surf to my web blog :: http://www.the-social-network.net/blog/view/79730/news-on-convenient-acne-no-more-methods
I've been exploring for a bit for any high quality articles or blog posts in this sort of space . Exploring in Yahoo I eventually stumbled upon this site. Studying this information So i'm glad to exhibit that I've an incredibly excellent uncanny feeling I came upon exactly what I needed. I most indubitably will make sure to don?t fail to remember this site and give it a glance on a constant basis.
ReplyDeleteFeel free to visit my homepage ... acne spot treatment
Hello everyone, i'm Linda Harry from United State i was diagnosed with Parkinson Disease for over 6 years which made me loose my job and my relationship with my Fiance after he discovered that i was having Parkinson, he departed from me, and i tried all my best to make him stays, but he neglected me until a friend of mine from UK told me Great healer, who will restore my life back with his powerful healing herbal medicine. then he sent me his email address to contact him- drimolaherbalmademedicine@gmail.com. and i quickly contacted him, and he said my condition can be solved, that he will treat the disease immediately only if i can accept trust on him and accept his terms and condition, i Agreed because i was so much in need of help by all means, so i did all he instructed me to do. And surprisingly after two weeks, He sent me a text, that i should hurry up to the hospital for a checkup, which i truly did, i confirm from my doctor that i am now ( PARKINSON NEGATIVE) my eyes filled with tears and joy, crying heavily because truly the disease deprived me of many things from my life, This is a Miracle, dr imoloa also uses his powerful herbal medicine to cure the following diseases: lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis A.B.C., syphilis, diarrhea, HIV/AIDS, Huntington's Disease, back acne, Chronic renal failure, addison disease, Chronic Pain, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, fungal nail disease, Lyme Disease, Celia disease, Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis , Multiple Sclerosis, Muscular Dystrophy, Rheumatoid Arthritis, Alzheimer's Disease, parkison disease, vaginal cancer, epilepsy, Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumour, Malignant, Bruxism, Bulimia, Cervical Disk Disease, cardiovascular disease, Neoplasms, chronic respiratory disease, mental and behavioural disorder, Cystic Fibrosis, Hypertension, Diabetes, asthma, Inflammatory autoimmune-mediated arthritis. chronic kidney disease, inflammatory joint disease, impotence, feta alcohol spectrum, Dysthymic Disorder, Eczema, tuberculosis, Chronic Fatigue Syndrome, constipation, inflammatory bowel disease, bone cancer, lung cancer. contact him on email- drimolaherbalmademedicine@gmail.com. and also on whatssap- +2347081986098
ReplyDelete